Medication-Assisted Treatment (MAT) programs for Opioid Addiction

Buprenorphine Injections
Buprenorphine injections are a pharmaceutical intervention used primarily in the treatment of opioid addiction. Buprenorphine is a partial opioid agonist, which means it activates the opioid receptors in the brain to a lesser degree than full agonists like heroin or methadone. This action helps to alleviate cravings and withdrawal symptoms associated with opioid dependence, but with a lower potential for abuse and overdose.
The medication is available in various formulations, including sublingual tablets and films, but the injectable form specifically offers several benefits. Buprenorphine injections are long-acting, typically administered once a month, which can improve adherence to the treatment regimen by eliminating the need for daily dosing. This can be particularly beneficial for patients who may struggle with medication compliance or those who prefer not to take daily medication.
There are two main types of buprenorphine injections: Sublocade and Brixadi. Sublocade is administered once monthly, while Brixadi can be administered weekly or monthly, depending on the treatment plan. These injections must be administered by a healthcare provider in a clinical setting.
The effectiveness of buprenorphine injections in reducing opioid use and improving treatment outcomes has been demonstrated in various studies. The medication is generally well-tolerated, although some common side effects may include injection site reactions, headache, nausea, and constipation. Importantly, buprenorphine has a "ceiling effect," which means that beyond a certain dose, no additional increase in effect is observed, reducing the risk of respiratory depression, a serious risk associated with many other opioids.
Buprenorphine injections are part of a comprehensive treatment plan that includes counseling and support for individuals with opioid use disorder. This integrated approach is essential for addressing the psychological, social, and behavioral aspects of addiction, thereby enhancing the overall effectiveness of the medication and improving recovery outcomes.


Methadone
Methadone is a synthetic opioid medication that plays a crucial role in the treatment of opioid addiction, particularly heroin and other opioids. As a full opioid agonist, methadone mimics the effects of opioids at a slower, more controlled rate, which helps to reduce cravings and withdrawal symptoms without providing the euphoric high associated with opioid abuse.
Methadone is used primarily in medication-assisted treatment (MAT) programs for opioid addiction. Its administration is tightly regulated; patients typically receive the medication through a structured program at specialized clinics known as methadone clinics. These programs require patients to visit the clinic daily to receive their dose under the supervision of medical staff, ensuring both the safety of the patient and adherence to the treatment regimen.
The effectiveness of methadone in treating opioid addiction lies in its pharmacological action. It binds to the same opioid receptors in the brain as other opioids, helping to ease withdrawal symptoms and mitigate the physical discomfort associated with recovery. Moreover, methadone’s long half-life allows for once-daily dosing, which helps maintain stable drug levels in the blood and reduces the physiological urges that drive addictive behaviors.
Methadone treatment is often long-term, sometimes extending over several years or indefinitely, as abrupt discontinuation can lead to severe withdrawal symptoms. The dosage of methadone is carefully managed and individually tailored to each patient's needs, with periodic adjustments made based on their response to the treatment.
Aside from its physiological benefits, methadone treatment is usually accompanied by comprehensive support services, including counseling, behavioral therapies, and support groups. These services are integral to addressing the psychological and social dimensions of addiction, thereby enhancing the overall effectiveness of the treatment and aiding long-term recovery.
While highly effective, methadone use comes with its own risks, such as the potential for abuse, dependency, and side effects like sedation, respiratory depression, and cardiac issues. Therefore, its use is closely monitored by healthcare providers to mitigate these risks, making it a controlled but critical component of opioid addiction treatment strategies.

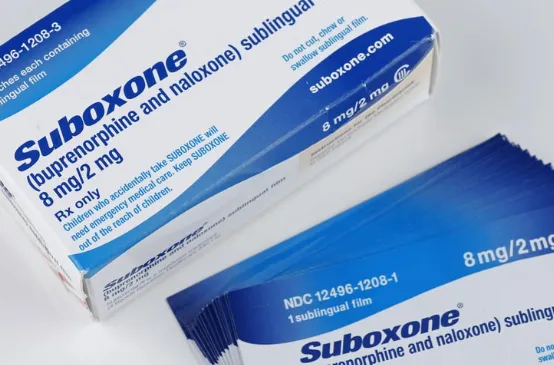
Suboxone
Suboxone is a medication used in the treatment of opioid addiction that combines two active ingredients: buprenorphine and naloxone. Buprenorphine is a partial opioid agonist, which means it activates opioid receptors in the brain but produces a much milder effect compared to full agonists like heroin or methadone. Naloxone, on the other hand, is an opioid antagonist that blocks the effects of opioids at receptor sites and is included primarily to prevent misuse of the medication.
Suboxone is administered primarily in a sublingual form, either as a film or tablet that dissolves under the tongue. This method of administration helps in maintaining consistent levels of medication in the body, aiding in managing withdrawal symptoms and reducing opioid cravings without the euphoric high associated with opioid abuse.
The combination of buprenorphine and naloxone in Suboxone is particularly effective for outpatient treatment of opioid addiction. Buprenorphine's partial agonist properties allow it to suppress withdrawal symptoms and cravings effectively, while naloxone acts as a safeguard against misuse of the medication, as it can precipitate withdrawal symptoms if the medication is injected rather than taken sublingually as prescribed.
Treatment with Suboxone typically begins with an induction phase, where the correct dose to stabilize the patient is determined under medical supervision. This is followed by a maintenance phase, where the dose may be adjusted to the minimum effective level that prevents opioid use and allows the patient to engage effectively in daily activities. The duration of treatment varies, ranging from several months to potentially lifelong maintenance, depending on the individual's needs and response to treatment.
Suboxone therapy is most effective when combined with comprehensive addiction treatment services, including counseling and behavioral therapies. These interventions address the psychological and behavioral aspects of addiction, helping patients develop coping strategies to manage triggers and cravings and ultimately leading to more successful long-term recovery outcomes.
While Suboxone is a powerful tool in the management of opioid addiction, it also carries some risks, such as the potential for abuse, though it is generally lower compared to other opioids. Side effects may include nausea, headache, sweating, and potential withdrawal symptoms if the medication is stopped abruptly. Careful management and monitoring by healthcare providers are essential to maximize the benefits of Suboxone in treating opioid addiction while minimizing potential risks and side effects.
What is Medication-Assisted Treatment (MAT) programs for Opioid Addiction
Medication-Assisted Treatment (MAT) programs are a clinical approach to treating substance use disorders, particularly opioid addiction, combining pharmacological interventions with behavioral therapies. MAT is designed to address the whole spectrum of addiction through a comprehensive and tailored approach that includes FDA-approved medications, counseling, and behavioral modifications to treat the physical, psychological, and social aspects of addiction.
Pharmacological Treatment:
MAT uses specific medications that act on the same opioid receptors in the brain as the addictive drug but are safer and less likely to produce the harmful behaviors that characterize substance use disorders. The most common medications used in MAT for opioid addiction include:
Methadone: A long-acting opioid agonist that reduces cravings and withdrawal symptoms, administered daily under supervised conditions at specialized clinics.
Buprenorphine: A partial opioid agonist that lowers cravings and withdrawal symptoms with a lower risk of euphoria and dependency, available through prescription from certified doctors.
Suboxone: An opioid antagonist that blocks the effects of opioids at receptor sites and is used primarily for preventing relapse rather than for withdrawal symptoms. It can be administered as a pill or as a monthly injection.
Behavioral Therapies:
Behavioral interventions are a core component of MAT, as they help patients change their thinking and behaviors related to drug use. Therapies may include:
Cognitive Behavioral Therapy (CBT): Helps patients recognize, avoid, and cope with the situations in which they are most likely to use drugs.
Motivational Interviewing: Increases an individual’s motivation to change behavior and engage in treatment.
Group Therapy: Provides peer support and reinforces behaviors conducive to recovery.
Goals of MAT:
The primary goals of MAT are to improve patient survival, increase retention in treatment, decrease illicit opiate use and other criminal activity among people with substance use disorders, and increase patients' ability to gain and maintain employment. Moreover, MAT aims to improve birth outcomes among women who have substance use disorders and are pregnant.
Integrated Care:
MAT programs are often integrated within community settings, which allows for more coordinated care involving mental health specialists, medical professionals, and social services to provide a holistic approach to treatment. This integration helps address not only the addiction itself but also related health conditions including HIV/AIDS, hepatitis, and other conditions often associated with substance abuse.
Effectiveness and Acceptance:
Research shows that MAT can effectively sustain recovery and prevent overdose, with the medications providing a controlled level of the drug to the patient, which helps to reduce misuse of opioids. Despite its demonstrated effectiveness, there's sometimes stigma associated with MAT as some perceive it merely as replacing one drug with another. Education and awareness are crucial to increasing its acceptance and use as an essential component of the public health approach to managing the opioid crisis.
Overall, MAT programs represent a progressive and evidence-based approach to addiction treatment, emphasizing that addiction is a medical condition that can be effectively treated with a combination of medical and behavioral interventions.

Contact Us
1-888-996-LWIN (5946)
245 5th Avenue, 3rd Floor, New York, NY 10016
Monday - Friday: 10:00 am - 8:00 pm
Saturday & Sunday: 10:00-5:00 pm
© Copyright 2024 Dr. Lwin Medical, PLLC. All rights reserved. SMS Policy | Terms and Conditions | Privacy Policy